The following steps are performed during the surgery:
- The healthcare provider will ask you to remove your clothes, jewellery or any item that interferes with the surgical procedure. You will have to wear a gown provided by the hospital for the surgery.
- A urine catheter will be inserted into your bladder to collect urine and empty your bladder and an intravenous (IV) line will be placed in your arm or hand to provide you with necessary fluids and medicines.
- Your heart rate, breathing, oxygen level and blood pressure will be continuously monitored during the surgery.
- To begin the surgery, excess hairs would be shaved off from the site of the surgery and it will be cleaned with an antiseptic solution.
- You will be given general anaesthesia for the surgery.
- To get your head into the right position for the surgery, a healthcare practitioner will secure your head in a specialised holder device, such as a Mayfield three-pin head holder. The device may be attached to the operating table already.
- Next, the surgeon will make an incision on the skin of your skull. The type of incision will be decided on the basis of the affected area and the type of craniotomy - a smaller incision is made in endoscopy craniotomy.
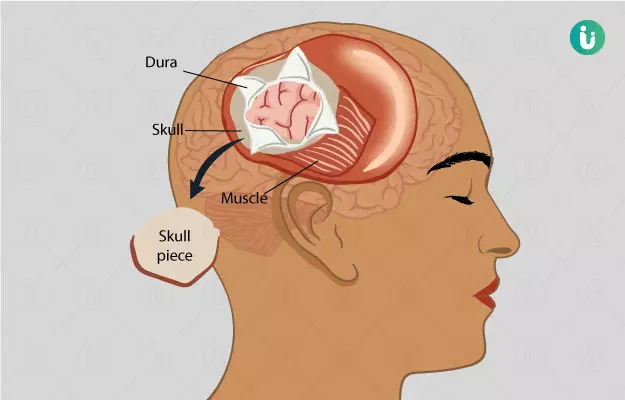
- After the incision, the surgeon will then part or pull up your scalp.
- To control bleeding caused due to the incision, he/she will place a surgical clip on your scalp.
- Next, A medical drill and saw will be used to make burr holes and cut the bone in your skull, respectively.
- The surgeon will then remove and save the bone flap.
- The dura mater will be detached from the bone and cut to expose the brain.
- Depending on the condition, the surgeon will further monitor and perform the surgery. For example, a monitor will be placed inside the brain tissue to check the pressure inside the brain.
- After the surgery is done, the layers will be sewed (sutured) together.
- The bone flap will be attached again using plates, suture or wires.
- The scalp will be closed with suture or surgical staple.
- Next, the area will be covered with sterile bandage or dressing.
Some types of craniotomy are as follows:
- Craniectomy: In this type of surgery, the bone flap is not replaced immediately. After a few weeks or months, the removed part is replaced using a metal plate, synthetic material or the person’s original bone. In some cases, the bone flap portion is removed permanently.
- Image-guided craniotomy or stereotactic craniotomy: This surgery is performed using a computer and various imaging procedures, such as magnetic resonance imaging (MRI) or computed tomography (CT) scan. The three-dimensional images help to locate the exact area in the brain that is to be treated.
- Endoscopy craniotomy: In this surgery, an endoscope is used to visualize the area in the brain. It involves the insertion of a lighted scope with a camera through a small hole in the skull.
- Minimally invasive supra-orbital craniotomy: This type of surgery involves an incision (cut) within the eyebrow region. It causes lesser pain, minimizes scarring and enables speedy recovery.
- Orbitozygomatic craniotomy: This surgery includes temporary removal of the bone from the cheek and the eye socket (orbit) area. It gives better access to the brain and minimizes brain damage.
- Extended bifrontal craniotomy: In this surgery, an incision is made behind the hairline.
- Translabyrinthine craniotomy: In this surgery, the bone behind the ear is removed. This surgery may cause permanent hearing loss.
- Retro-sigmoid ‘keyhole’ craniotomy: In this surgery, an incision is made behind the ear. It minimizes pain and scarring and improves recovery.
After the surgery
After the surgery is performed, you will be shifted to a recovery room and then to the intensive care unit (ICU). In the ICU, your head will be kept raised to prevent brain swelling, and your intracranial pressure will be monitored. The healthcare practitioner will give you medicines to lessen your brain swelling.
Gradually, the devices used to measure intracranial pressure will be removed. Once you are stable, you will be shifted to your hospital room. You will still have the urinary catheter and oxygen support for a few more days or till your discharge. This support will be taken off too before you are discharged.
To prevent pneumonia, you will be taught deep-breathing exercises to get back your lung function.
Your brain function will be checked by asking you some questions to check your awareness level, checking your pupil and asking you to move your arms and legs.
Based on your condition after surgery, your diet may vary. Liquids are usually given a few hours after surgery, and you are gradually transitioned to more solid foods as you start to tolerate them.
When you are able to, you will be asked to walk around a bit. A physical therapist will initially help you with this. Once you are able to walk, the urine catheter would be removed too. Inform your doctor if you have any symptoms of urine infection once the catheter is removed. The physical therapist will check your balance, movements and strength. You may be shifted to a rehabilitation facility till you regain your strength or the therapist will suggest some exercises to regain your strength.
Before discharge from the hospital, the healthcare practitioner will give you instructions for home care and arrange your follow-up meetings.