A corneal transplant or keratoplasty is a surgical procedure to replace the diseased or damaged cornea with a healthy donated cornea (permission is given by the donor before death or, more commonly, by the family).
The cornea is a clear, dome-shaped front portion of the eye. It consists of three main layers and two thin layers between them. Cornea prevents the entry of germs, dirt, damaging ultraviolet (UV) light, and other particles into the eye. It also helps to focus the light that enters the eye and makes the vision clear.
If the cornea gets damaged, it may change its shape or become cloudy and opaque. This may lead to blindness.
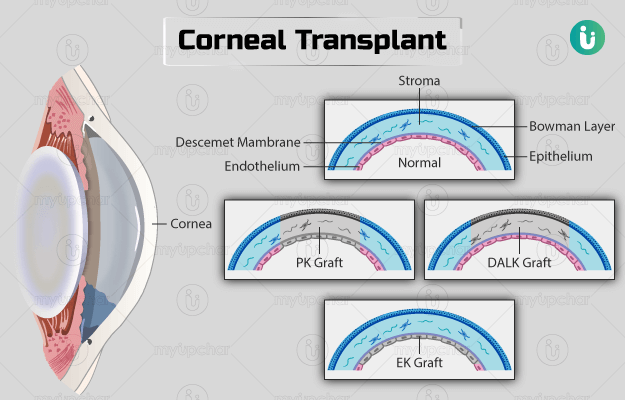
The cornea consists of five layers of cells. The outermost layer is the epithelium that acts as the main barrier to protect the eye. The epithelium is followed by a layer of tough tissue called Bowman’s layer, which helps give cornea it's unique shape. The Bowman’s layer is followed by stroma, Descemet’s membrane (DM), and the innermost layer known as the endothelium. Stroma contributes to about 95% of the total corneal thickness. Descemet’s membrane is the strongest layer in the cornea. The innermost endothelial layer consists of a single cell layer that maintains transparency or clarity of the cornea.
Based on the layers of the cornea that are damaged and replaced, the surgeon will recommend one of the following types of keratoplasty:
- Penetrating keratoplasty: Entire cornea
- Anterior lamellar keratoplasty: This type of keratoplasty consists of the following subtypes with each listing the layer to be removed:
- Bowman’s layer transplant: Bowman’s layer
- Superficial anterior lamellar keratoplasty: Superficial layers of the stroma
- Deep anterior lamellar keratoplasty: Stroma
- Posterior lamellar keratoplasty/endothelial keratoplasty: The type can be further divided into the following subtypes:
- Descemet’s membrane endothelial keratoplasty: Endothelium and DM (replaced by donor endothelium and DM)
- Descemet’s stripping endothelial keratoplasty: Endothelium and DM (replaced by donor DM and endothelium and inner layers of stroma)
Keratoprosthesis is a type of keratoplasty that replaces the entire cornea with an artificial implant.