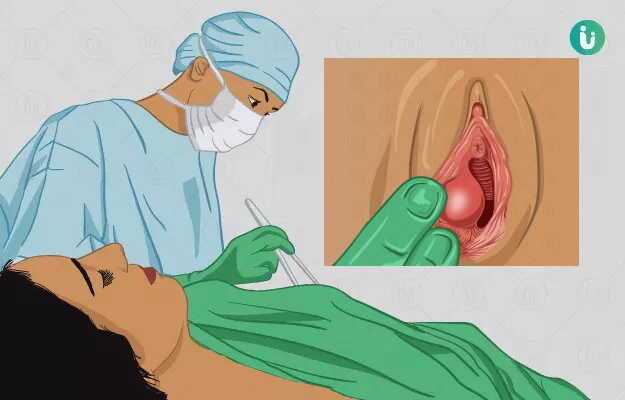
Bartholin cyst surgery is a minor surgical procedure to treat a Bartholin cyst in females. When the Bartholin gland is blocked it forms a Bartholin cyst.
The reason for surgery is the onset of painful symptoms caused by the cyst.
The procedure is a minor one and the patient is admitted in the morning and discharged by the evening (day-care admission). Aftercare is important to prevent recurrence. The period of wound healing varies from two to four weeks depending on the type of procedure performed.