Summary
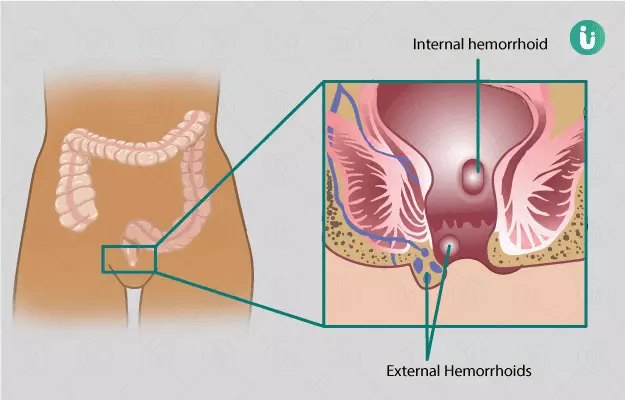
A haemorrhoidectomy is a surgery to remove severe haemorrhoids (piles) that are associated with uncomfortable symptoms like pain, itching, and lumps around the anus. A haemorrhoidectomy can be performed with closed, open, stapled or rubber band ligation techniques. The surgery requires the administration of a sedative (medicine that induces sleep) and takes not more than 45 minutes to complete.
This surgery is mainly done to provide relief from symptoms of inflamed haemorrhoids. However, the surgery is associated with a high rate of complications such as pain and bleeding from the anus, which may persist for a few weeks. The average recovery time after the surgery is 2 to 3 weeks.