Ever spotted stubborn dark patches on your face – those brownish or grayish-brown marks often on your forehead, cheeks, or upper lip? That's likely melasma, a common skin condition that can really bother people. It's especially common for women, particularly those with darker skin, and its unpredictable nature can make it tricky to deal with.
Melasma is truly widespread. Globally, it affects millions, with a higher prevalence in populations with Fitzpatrick skin types III-VI (people with olive, brown, or darker skin tones). For instance, studies suggest that in regions like Southeast Asia, Latin America, and India, melasma can affect up to 25-30% of women in certain age groups. In the general U.S. population, its prevalence is estimated to be around 5-6 million people. This makes it one of the most common pigment disorders.
We know a few big reasons why melasma pops up. Sun exposure is a major culprit; UV rays kick your skin's pigment-making cells into overdrive. Then there are hormone changes, which is why many women get it during pregnancy (often called the "mask of pregnancy") or when taking birth control. Your genetics also play a part – if melasma runs in your family, you might be more prone to it. Sometimes, even skin irritation can trigger it.
Even with these known triggers, melasma remains a bit of a mystery. Why does it show up for some and not others? Why is it so hard to treat and why does it keep coming back? Dermatologists are always looking for more answers. Recently, a fascinating question has come up: Could something as basic as iron deficiency be involved in this puzzling skin condition? In this article, we'll dive into this idea, simply exploring what iron is, how your skin gets its color, and what the science currently tells us about any connection between low iron and melasma.
- Understanding Iron and Its Vital Role in the Body
- Where Melasma Happens
- How Melasma Develops
- What Do Studies Say?
- Clinical Implications and Practical Advice
- Treating Iron Deficiency
- Complementary Skincare Approaches You Can Try at Home
- Is Treating Iron Deficiency a Melasma Cure?
- Summary
Understanding Iron and Its Vital Role in the Body
Before we delve into the potential link between iron and melasma, it's essential to grasp just how crucial iron is for our overall health. What exactly is iron? Simply put, iron is an essential mineral. This means your body cannot produce it on its own; you must obtain it through the foods you eat. Despite being a trace element, its functions are anything but small.
(Read More: Effective Home Remedies for Sun Tan Removal)
Key Functions of Iron in the Body:
The roles of iron are diverse and fundamental to life:
- Oxygen Transport (Hemoglobin): This is iron's most famous and vital job. Iron is a key component of hemoglobin, a protein found in your red blood cells. Think of hemoglobin as the tiny delivery truck that picks up oxygen from your lungs and transports it to every single cell, tissue, and organ in your body. Without enough iron, your body can't make enough healthy hemoglobin, leading to a shortage of oxygen delivery. This directly affects your energy levels and overall bodily function.
- Energy Production: Beyond oxygen transport, iron plays a critical role in the processes that generate energy within your cells. It's a vital part of many enzymes that help convert food into usable energy, meaning sufficient iron is necessary for you to feel energetic and perform daily tasks.
- Immune System Function: A robust immune system depends on iron. This mineral is crucial for the healthy development and proper functioning of various immune cells, which are your body's defenders against infections and diseases.
- Cognitive Function: Iron supports brain health and development. Adequate iron levels are linked to better concentration, memory, and overall cognitive performance.
DNA Synthesis: Iron is involved in the creation of DNA, the genetic material in every cell, which is essential for cell growth, division, and repair throughout your body.
Iron Deficiency (ID) vs. Iron Deficiency Anemia (IDA)
It's important to understand the difference between iron deficiency and iron deficiency anemia, though they are related:
- Iron Deficiency (ID): This is when your body's stores of iron are low, even if you don't yet have full-blown anemia. It's often detected by checking ferritin levels, which reflect your stored iron.
- Iron Deficiency Anemia (IDA): This is a more advanced and severe stage. Here, your iron levels are so low that your body cannot make enough healthy red blood cells, leading to a reduced ability to carry oxygen.
(Read More: What is Double Chin, How to Remove Double Chin)
Common Symptoms of Iron Deficiency
When your body doesn't have enough iron, you might experience a range of symptoms, including profound fatigue, general weakness, pale skin, shortness of breath, dizziness, cold hands and feet, brittle nails, unusual hair loss, and sometimes even pica (a strange craving for non-food items like ice or dirt).
Iron deficiency is not uncommon; in fact, it's one of the most widespread nutritional deficiencies globally, particularly affecting women of childbearing age due to menstruation. Given its extensive roles throughout the body, it's natural to wonder if a lack of this vital mineral could have an impact on a condition like melasma.
Where Melasma Happens
To understand any potential link between iron deficiency and melasma, we first need to grasp the basics of how our skin gets its color. Our skin is made up of several layers, but for melasma, we mainly focus on the top layer, called the epidermis, and sometimes the layer just beneath it, the dermis. Melasma typically involves changes happening in these layers.
Melanin
The color of your skin, hair, and eyes comes from a natural pigment called melanin. Melanin is what gives each of us our unique hue, from very pale to very dark. There are two main types of melanin:
- Eumelanin: This produces brown and black colors. Melasma usually involves an increase in eumelanin.
- Pheomelanin: This produces red and yellow colors.
Melanocytes
Melanin is produced by specialized cells in our skin called melanocytes. These cells are located in the very bottom part of the epidermis, the top layer of your skin. Think of melanocytes as tiny factories responsible for creating all the pigment.
Inside these melanocytes, melanin is made and then packaged into small sacs called melanosomes. Once these melanosomes are full of pigment, they are transferred from the melanocytes to the surrounding skin cells, called keratinocytes. It's this transfer and the amount of melanin produced that ultimately determines your skin coloration.
(Read More: Ancient Beauty Secrets: Home Remedies for Glowing Skin)
Factors Influencing Melanin Production
Several factors can influence how much melanin your melanocytes produce:
- UV Radiation (Sunlight): This is by far the strongest trigger. When your skin is exposed to sunlight (specifically UV rays), it acts as a signal to your melanocytes to produce more melanin. This is your body's natural defense mechanism to protect against sun damage, which results in a tan. In melasma, these melanocytes become overly sensitive to sun exposure.
- Hormones: Hormones, particularly estrogen and progesterone (which fluctuate during pregnancy, and are present in birth control pills or hormone replacement therapy), can also stimulate melanocytes. This is why pregnant women often develop melasma.
- Genetics: Your genes play a significant role. If your family members have melasma, you may have melanocytes that are naturally more prone to becoming overactive.
- Inflammation: Any irritation or inflammation in the skin can sometimes lead to what's called post-inflammatory hyperpigmentation, where the skin darkens after an injury or irritation.
How Melasma Develops
In melasma, the melanocytes in affected areas become overly active and produce far too much melanin in response to triggers like sun exposure or hormonal changes. This excess melanin then accumulates in the epidermis, forming the dark patches (this is called epidermal melasma). Sometimes, the melanin can even drop down into the deeper layer of the skin, the dermis (called dermal melasma), making the condition even harder to treat. Recent research also suggests that an increase in blood vessels within the melasma lesions (a condition called vascularity) might also play a role in its development and persistence. Understanding these complex processes is vital as we now consider whether iron, an essential mineral, fits into this intricate picture.
(Read More: Benefits of Vitamin E for Skin to Make Skin Beautiful and Healthy)
Iron Deficiency and Melasma
With a clear understanding of what iron does for the body and how skin pigmentation works, we can now dive into the central question: Is there a connection between iron deficiency and melasma? It’s a fascinating area of study, but also one where the answers are not yet fully clear.
How Low Iron Affects Melanin Production?
Researchers have proposed several ways in which a lack of iron could potentially influence the development or severity of melasma. These are mostly theories based on what we know about iron’s roles in the body:
- Enzyme Activity: Iron is a crucial component, or "cofactor," for many enzymes that enable vital chemical reactions in our bodies. It is hypothesized that iron deficiency might affect the activity of certain enzymes involved in the melanin synthesis pathway – the complex series of steps your body takes to make pigment. For example, some enzymes involved in making melanin might rely on iron, and if iron is scarce, these enzymes might not work as efficiently or, conversely, might become overactive in an attempt to compensate, leading to imbalanced melanin production. However, direct strong evidence showing which specific enzymes in the melanin pathway are directly impacted by iron deficiency is still largely under investigation.
- Cellular Metabolism & Oxidative Stress: Iron deficiency affects the overall way your cells function and produce energy. When iron levels are low, it can lead to increased oxidative stress in the body. Oxidative stress is like a harmful imbalance where there are too many "free radicals" (unstable molecules) and not enough antioxidants to neutralize them. This stress can damage cells, and importantly for our discussion, it is known to stimulate the production of melanin. If iron deficiency causes more oxidative stress in skin cells, it could potentially trigger melanocytes to produce more pigment, contributing to melasma.
- Overall Skin Health and Oxygenation: Iron's primary role in carrying oxygen means that a deficiency could lead to less oxygen reaching skin cells. Healthy, well-oxygenated skin is important for its normal functions. Any disruption in oxygen supply or general skin health due to iron deficiency might indirectly impact the regulation of pigment production, making melanocytes more prone to overactivity when faced with triggers like sun exposure.
(Read More: Best fruits for glowing skin)
What Do Studies Say?
The scientific community is still working on understanding the direct link between low iron and melasma, and current research shows mixed results. Some studies, mostly observational ones, have found a possible connection. For example, research in different countries has shown that women with melasma sometimes have lower iron levels, especially lower levels of ferritin (which indicates your body's stored iron), compared to women without the condition. This suggests that if your body is low on iron reserves, it might make you more prone to melasma. There have also been a few small reports where melasma improved for some iron-deficient patients after taking iron supplements. However, these individual cases aren't strong enough proof that low iron directly causes melasma or that iron treatment will cure it.
On the flip side, other studies have found no clear difference in iron levels between people with and without melasma. This means if a link exists, it might not be strong or apply to everyone. These mixed findings can be due to various reasons, like how the studies were set up, the different groups of people included, how "iron deficiency" was defined, or how well other influencing factors were managed in the research.
Some research hints at a possible connection between lower iron levels (especially ferritin) and melasma, the scientific community has not yet firmly established iron deficiency as a direct, standalone cause of melasma. It's an area that continues to be investigated, and future, more robust research is needed to provide clearer answers.
Clinical Implications and Practical Advice
Given the ongoing research and the nuances of the potential link between iron deficiency and melasma, what does this mean for you, and what practical steps should you take?
(Read More: DIY Facial at Home: Your Complete Guide to Glowing Skin)
When to Consider Iron Testing for Melasma Patients:
While iron deficiency isn't a proven cause, it's a common condition that can affect overall health. Therefore, if you have melasma, it's reasonable to consider having your iron levels checked under certain circumstances:
- Persistent or Resistant Melasma: If your melasma is particularly stubborn and not responding well to conventional treatments, exploring all potential contributing factors, including nutritional deficiencies, can be a part of a thorough investigation.
- Symptoms of Iron Deficiency: If you experience any of the common symptoms of iron deficiency such as unusual fatigue, pale skin, weakness, shortness of breath, dizziness, cold hands or feet, or brittle nails, it's advisable to get your iron levels tested regardless of your melasma.
- High-Risk Groups for Iron Deficiency: If you fall into a group that is typically at higher risk for iron deficiency, testing is particularly important. This includes menstruating women (especially those with heavy periods), pregnant women, individuals following vegetarian or vegan diets (as plant-based iron is less easily absorbed), and those with certain digestive conditions that can affect nutrient absorption (like celiac disease or inflammatory bowel disease).
When to See a Doctor
It's really important to remember that you shouldn't try to diagnose or treat iron deficiency yourself. Only a healthcare professional can figure out if you're truly low on iron and guide you on how to fix it safely.
(Read More: Gluten and Gluten-Free Foods)
How Doctors Diagnose Iron Deficiency
If you or your doctor suspect you might have low iron, they'll likely order some simple blood tests. These usually include a Complete Blood Count (CBC), which checks your red blood cells. Crucially, they'll also test your serum ferritin (to see how much iron your body has stored), along with serum iron and transferrin saturation. These tests combined give your doctor a clear picture of your iron levels.
Treating Iron Deficiency
Once an iron deficiency is diagnosed, your doctor will work with you to create a personalized treatment plan. This plan often involves two main approaches:
Dietary Adjustments
A key part of your iron recovery plan will almost certainly involve making smart choices about the food you eat. While severe cases might need iron supplements (which your doctor will prescribe), a well-planned diet is the natural, ongoing way to rebuild your iron stores and maintain them. Think of food as your first line of defense and a powerful tool in your iron-boosting journey.
Your doctor will guide you on how to adjust your eating habits, focusing on foods naturally rich in iron. There are two main kinds of iron you get from food, and your body absorbs them differently:
- Heme Iron: The Easy Absorber This type of iron is found in animal products. It's the most easily absorbed by your body, meaning you get more iron from these sources. Good examples include red meat (like beef and lamb), poultry (chicken, turkey), and fish. Including these in your diet, if you eat meat, can give your iron levels a significant boost.
- Non-Heme Iron: The Plant-Powered Option Non-heme iron comes from plant sources. While it's not absorbed as easily as heme iron, it's still incredibly important and forms a large part of many healthy diets. You'll find it in foods like lentils, various kinds of beans (black beans, kidney beans, chickpeas), leafy green vegetables such as spinach and kale, fortified cereals, tofu, and many nuts and seeds.
(Read More: The Hydrafacial Revolution)
Boosting Your Absorption and Avoiding Blockers
Simply eating iron-rich foods is a great start, but how you combine them can make a big difference! Your body is clever, but it needs a little help to absorb non-heme iron effectively.
- Boost Absorption with Vitamin C: This is a super important tip! Vitamin C dramatically helps your body take in non-heme iron. So, try to eat foods rich in Vitamin C alongside your plant-based iron sources. Think about pairing lentils with bell peppers, or enjoying spinach with a squeeze of fresh lemon juice. Citrus fruits (oranges, grapefruits), tomatoes, and strawberries are also excellent sources of Vitamin C.
- Time Your Drinks: Be mindful of what you drink around meal times. Tea and coffee contain compounds called tannins that can actually block iron absorption, especially non-heme iron. It's often best to enjoy these beverages at least an hour before or after your main iron-rich meals.
- Watch Out for Calcium: Calcium, found in dairy products like milk, cheese, and yogurt, can also interfere with iron absorption. This doesn't mean you should avoid calcium – it's vital for bones! Instead, try to separate very high-calcium foods from your main iron-rich meals. For instance, have your yogurt as a snack between meals rather than with your iron-packed lunch.
- Prepare Your Grains and Legumes: Soaking, sprouting, or fermenting grains and legumes can help reduce phytates, natural compounds that can also hinder iron absorption. Cooking generally helps too.
(Read More: Fairer Skin for Men: A Male Guide to Brighter Complexion)
Iron Supplements
If changing your diet isn't enough, your doctor might prescribe iron supplements. These come in different forms, and your doctor will recommend the best type and dose for you. It's really important to follow their instructions, as taking too much iron or taking it incorrectly can lead to side effects like constipation, nausea, or an upset stomach. Never take iron supplements without your doctor's recommendation, as too much iron can actually be harmful.
Addressing the Root Cause
For some people, iron deficiency might be ongoing or severe. In such cases, your doctor will also look for and treat the underlying reason for your low iron. This could be things like very heavy menstrual bleeding, internal bleeding in your digestive system, or conditions that make it hard for your body to absorb nutrients.
(Read More: Anti acne diet: Foods to eat and diet plan)
Complementary Skincare Approaches You Can Try at Home
When managing a persistent condition like melasma, it's natural to explore various options, including gentle approaches you can try at home. While many traditional or popular home remedies exist, it's vital to remember that their effectiveness for melasma is generally based on individual experiences rather than robust scientific proof. These methods should always be seen as complementary and never as a replacement for professional medical advice or prescribed treatments from a dermatologist. Always have a conversation with your doctor or dermatologist before trying any new home remedy, especially if you have sensitive skin or other existing skin conditions.
Here are a few gentle home-based approaches that some individuals incorporate into their routine, along with important cautions:
Aloe Vera
Known for its soothing and potential healing properties, aloe vera contains compounds like aloin. Some preliminary research suggests aloin might have a very mild effect on reducing skin pigmentation.
- How to use: Apply fresh, pure aloe vera gel directly from the plant (or a reputable pure gel product) to the melasma patches before bedtime. Leave it on overnight and rinse in the morning.
- Caution: Aloe vera is generally well-tolerated, but always use pure gel and stop immediately if you notice any irritation, redness, or itching.
(Read More: Diet For Skin Whitening For Glowing Skin)
Turmeric Paste
This popular spice contains curcumin, a compound known for its anti-inflammatory and antioxidant properties. Some scientific studies are exploring if curcumin could also play a role in reducing melanin production.
- How to use: Mix turmeric powder with a small amount of milk, yogurt, or gram flour to form a smooth paste. Apply it evenly to the melasma patches, leave it on for about 15-20 minutes, then rinse thoroughly with lukewarm water.
- Caution: Turmeric can temporarily leave a yellow stain on the skin. Always do a small patch test on an inconspicuous area first to check for skin reaction and staining. Like many natural ingredients, turmeric can increase photosensitivity in some individuals, so strict sun protection is essential after use.
Apple Cider Vinegar (ACV) Diluted Solution
Some people believe the mild acidity (acetic acid) in apple cider vinegar might act as a very gentle exfoliant or mild bleaching agent, potentially helping to lighten superficial dark spots over time.
- How to use: Always dilute apple cider vinegar by mixing equal parts ACV and water (e.g., 1 tablespoon ACV with 1 tablespoon water). Apply this diluted solution carefully to the melasma patches with a cotton ball, allow it to dry, and then rinse your face with lukewarm water after 5-10 minutes. Do this once a day at most.
- Caution: Extreme caution is needed. ACV is acidic and can cause significant skin irritation, dryness, and even chemical burns, especially on sensitive skin or if not properly diluted. Always perform a patch test on a small, hidden area of skin at least 24 hours beforehand. Avoid sun exposure immediately after using ACV, as it can increase your skin's sensitivity to the sun.
(Read More: Which Fruits Should Be Part of Your Skincare Diet?)
Important Considerations for Any Home-Based Approach
Even when considering gentle home-based approaches, remember:
- Patience is Key: Any visible results, if they occur, will be extremely slow and subtle. These are not quick fixes.
- Not a Root Cause Solution: These approaches do not address the underlying causes of melasma, such as sun exposure, hormonal changes, or genetic predispositions.
- Sun Protection is Paramount: Regardless of any home remedies or medical treatments you use, strict and consistent sun protection remains the single most critical step in managing melasma and preventing its worsening.
- Stop if Irritated: If you experience any redness, itching, burning, excessive dryness, or worsening of your melasma, stop using the remedy immediately and consult your doctor. What works for one person may not work for another, and individual skin reactions can vary widely.
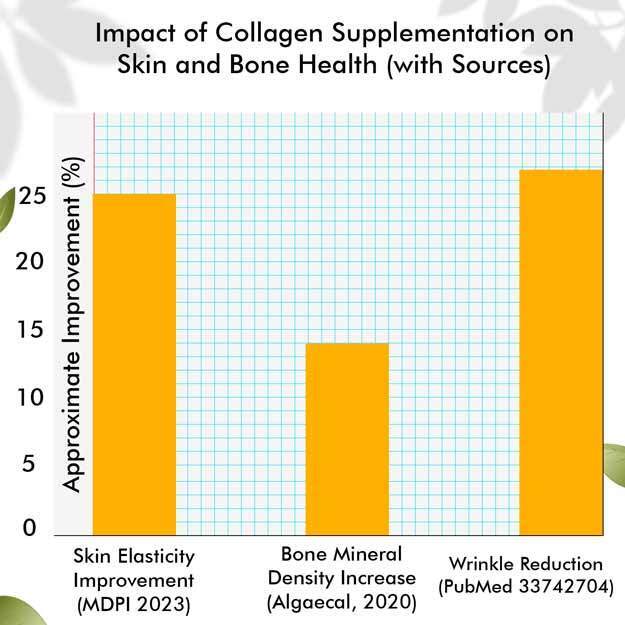
(Read More: From Skincare to Diet: How To Boost Collagen Naturally)
Is Treating Iron Deficiency a Melasma Cure?
It's vital to manage expectations here. While addressing an iron deficiency is essential for your overall health and well-being, it is highly unlikely to be a standalone cure for melasma. Melasma is a complex condition driven primarily by sun exposure and hormonal factors, with genetic predisposition playing a significant role.
Strategic Planning
The most effective management of melasma nearly always requires a multi-pronged strategy that includes:
- Strict Sun Protection: This is paramount. Daily use of broad-spectrum sunscreen (SPF 30 or higher), wearing wide-brimmed hats, and seeking shade are non-negotiable.
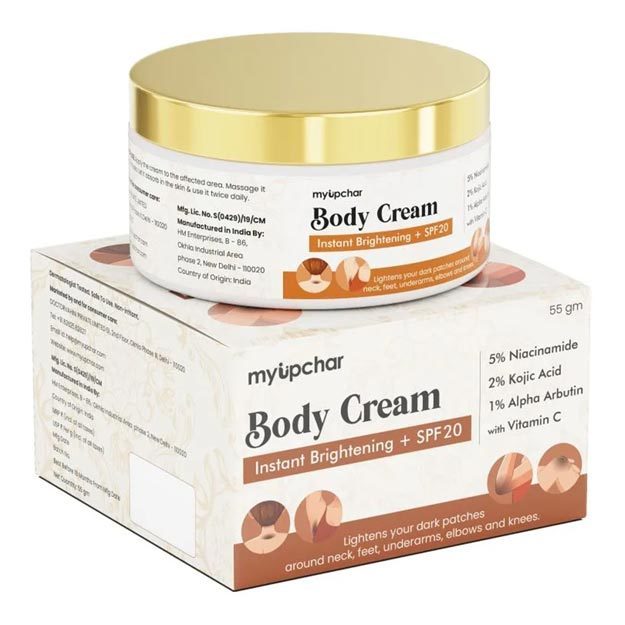
- Topical Treatments: These often include prescription creams containing ingredients like hydroquinone (which lightens dark spots), retinoids, azelaic acid, or kojic acid.
- Oral Medications: In some cases, a doctor might prescribe oral medications like tranexamic acid, but this is done under strict medical supervision due to potential side effects.
- In-office Procedures: Chemical peels or certain types of laser therapy might be considered, but these must be performed with extreme caution by an experienced dermatologist, as they can sometimes worsen melasma if not done correctly.
- Hormonal Evaluation: For women, a discussion about hormonal birth control or hormone replacement therapy might be necessary.
Potential Indirect Benefit
If an iron deficiency contributes to overall systemic health issues, fatigue, or increased oxidative stress, correcting it might indirectly support the body's ability to heal and respond better to other melasma treatments. It could potentially help improve the overall health of the skin, making it more resilient. However, this is more of a supportive role rather than a primary treatment for the pigment disorder itself.
In essence, while ensuring optimal iron levels is a cornerstone of good health, approach it as part of a comprehensive health strategy rather than a sole solution for melasma. Your healthcare provider is your best resource for personalized diagnosis and treatment.
(Read More: 5 Common Skin Problems and How to Solve Them Naturally)
Summary
As we've journeyed through this article, we've explored melasma, a common and often challenging skin condition characterized by those stubborn dark patches on the face. We've seen how factors like sun exposure, hormonal changes, and genetics are its primary drivers, affecting millions worldwide and significantly impacting their well-being.
We then delved into the crucial role of iron in your body, from carrying oxygen to boosting energy. While iron deficiency is a widespread issue, the scientific connection between low iron levels and melasma remains complex. Some studies suggest a possible link, but strong, direct proof that iron deficiency causes melasma is still lacking. Research is ongoing, and more robust studies are needed to fully understand any potential connection.
Ultimately, while addressing iron deficiency through a healthy diet and, if needed, supplements under a doctor's guidance is vital for your overall health, it's crucial to understand it's not a standalone cure for melasma. Effective management of melasma relies on a comprehensive strategy, with strict sun protection being paramount. This multi-pronged approach, which may also include topical treatments and professional procedures, remains the most effective way to manage this complex skin condition. Always consult your healthcare provider for personalized diagnosis and treatment for both iron deficiency and melasma.
Doctors for Melasma and Iron Deficiency: Unraveling a Complex Connection in Skin Pigmentation

Dr. Ashish Mishra
Dermatology
4 Years of Experience
Dr. Divyanshu Srivastava
Dermatology
10 Years of Experience

Dr. G.ARUN
Dermatology
6 Years of Experience